Quick summary:
- Some alternative and integrative doctors report a connection between root canals and cancer in the patients that they treat.
- They consider root canal treated teeth to be a burden on the immune system. The reasoning is that there are too many “nooks and crannies” where bacteria can hide, making it difficult to sterilize a tooth.
- Conventional dentists and endodontists say that properly treated root canals are not an issue at all… and that root canals are not linked to cancer, nor disease anywhere else in the body.
- While root canals have not been formally linked to cancer, there IS evidence that they could promote disease in other parts of the body.
- The research on cancer and root canals is also limited… so the possibility still exists.
- Multiple studies found some degree of infection in 50-90% of intact root canal treated teeth, when examined in patients and cadavers. Another showed infection in 86% of root canal treated teeth, even when the procedure was performed carefully.
- Root canal treatments can also differ greatly, ranging from poorly done, to very thoroughly done… and everything in between. Root canals that were not treated carefully could be at greater risk of being an immune burden.
- And overall, if you have a root canaled tooth, there is a good chance that it was treated in a “less than optimal” manner… especially if it was done by a general dentist.
- Root canaled teeth can also have infections, even when it’s not detected by x-ray. This could be worse if the dentist is using older x-ray technology.
- Based on the evidence that is available, there’s a greater than a 50% chance, that your root canal treated tooth is a burden on your immune system… even if the initial treatment was done carefully.
- So if you are fighting cancer and have root canaled teeth, it’s important to consider a variety of factors before deciding on your root canaled teeth. Potential solutions include extraction, or re-treatment with “apical surgery.”
When you are healing from cancer, you want every anticancer variable on your side. One of these factors is your oral health.
People often ask me if they should remove their root canal treated teeth when trying to heal from cancer. Some of you may have also read about the “dangers of root canals.”
But when you look into the root canal debate, you’ll see that it’s very a polarizing topic.
One side of the debate says that all root canals are dangerous because they are an immune burden….
The other side says it’s a myth…
So what’s the whole story? Should you get your root canals extracted?
We’ll examine the facts today, so that you can make the best decision for your case.
Root Canal Dangers?
The movement against root canals started with a dentist and nutrition researcher named Weston A. Price. Dr. Price traveled the world studying traditional cultures, and how they were affected by a “civilized diet” high in refined foods.

Dr. Weston A. Price
Dentist and Nutritional Researcher
Dr. Price found that switching to a “civilized diet” caused narrowing of the face, crowded dental arches, crowded teeth, increased tooth decay, and reduced immunity to disease.
(Photos from: Price, W. (2008). Nutrition and physical degeneration. Lemon Grove, CA: Price-Pottenger Nutrition Foundation.)
But beyond nutrition, Price also studied the health effects of root canal treated teeth [1]. In his experiments, he prepared root tip fragments of root canal treated teeth, and healthy teeth. Then he implanted them into rabbits (under their skin) to see how it would affect their health.
The healthy teeth didn’t create any issues in these rabbits. But when the root canaled teeth were implanted, the rabbits became ill. These rabbits often developed the same health issues as the person who donated their root canaled tooth for research.
The argument AGAINST root canal treatments is based on these concepts:
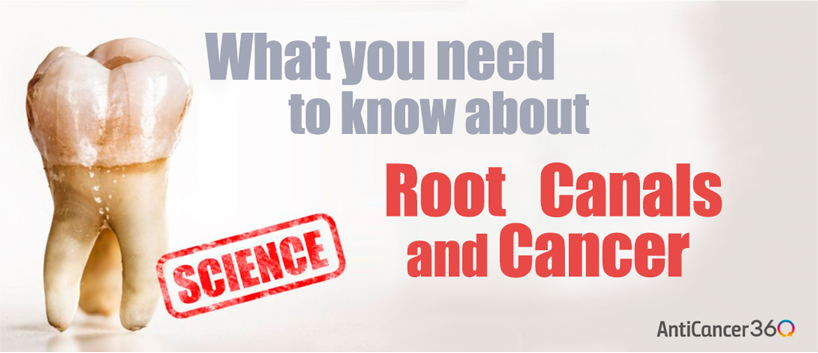
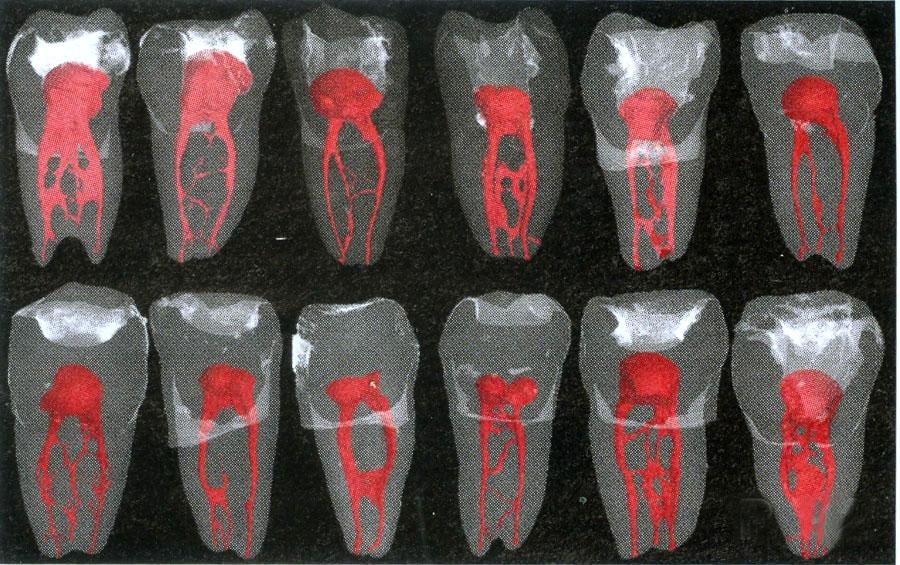
- Bacteria In Dentinal Tubules: Teeth are porous, with extensive networks of tunnels called “dentinal tubules.” When a tooth still is in the person’s mouth, it’s very difficult (some say impossible) to kill all of the bacteria in these microscopic tunnels.
- Accessory Canals: Besides the main canals, teeth also have smaller “accessory canals.” These are out of the reach of the tools used in a root canal procedure. This makes it a place where bacteria can persist.
- Periodontal Ligaments: Bacteria can infect the ligaments that hold the tooth to the bone. The bacteria migrates from the accessory canals mentioned above, or from the opening at the root of the tooth (due to a poor seal during root canal treatment.)
- Devitalized Teeth: When the nerves and blood vessels are removed during a root canal, it is no longer “alive.” This also means the immune system can no longer access the tooth. Because of this, and the leftover bacteria, root canal treated teeth are thought to be a point of low grade infection in your body.
- Immune Burden: The bacteria harbored in the root canaled tooth are an overall immune burden. They can also spread to, and affect other parts of your body.
Ultimately, if a root canaled tooth is harboring significant bacteria, it is thought to contribute to cancer (and other diseases) because of its burden on the immune system. When your immune system is overworked, it has less resources to deal with any cancer cells that may be multiplying in your body.
Affecting The Acupuncture Channels
Some health practitioners and holistic dentists also talk about the effects of a “dead” or missing tooth on the body’s acupuncture channels. Certain teeth are also thought to be correlated to different organs in the body.
Though this in itself is a controversial topic, this idea relates to two possible concepts.
The first is the electrical current that is generated when teeth hit each other (i.e. when you bite or chew.) This is referred to as a “piezoelectric effect, [2]” and it also happens when pressure is applied to the bone underneath the tooth.
These electrical currents are thought to affect the acupuncture channels, and the system of connective tissues that are everywhere in your body (i.e. fascia). [3][4][5][6][7] The fascia system is electrically conductive and is thought to be like a “second nervous system” in some senses.
Some say that “dead teeth” are unhealthy because don’t generate this electricity… But this is likely incorrect. “Dead” or “devitalized” root canal treated teeth should still generate piezoelectricity [8] (though it’s not clear to what extent compared to healthy teeth.)
But the bigger concern is the body constantly diverting blood flow and resources, to quarantine an infected root canal (we will discuss in more detail later.) This could also affect the electrical balance in the acupuncture channels, as your body depends partly on electro-chemicals (acetylcholine) to sustain circulation. [9][10]
Ultimately in acupuncture theory… disturbances in the energy channel, can disturb blood circulation/ microcirculation to other areas of the body. And because everything in your body is transported by blood and fluids, this can also affect the flow of nutrients, immune cells, oxygen, pH balancing factors, as well a your body’s own detoxification chemicals (glutathione, glucuronic acid etc…).
Most importantly, a disturbance to one part of the body can affect a totally different part of the body (see videos below.)
Interesting Note: Be sure to watch video 2, starting at 7:30… though the end of video 3… 🙂 Many scientists and doctors wonder why people can be so distrusting of conventional medicine at times. They also wonder why people are so obsessed with natural medicine “when there’s little scientific proof.” The clip above shows exactly why, and illustrates the need for science and medicine to “integrate” from both sides (i.e. because natural medicine is far from perfect also.)
So ultrasound energy can affect acupuncture channels and affected tissues in totally different areas of the body.
Electricity has also been traditionally thought to affect acupuncture channels, and change blood circulation patterns when used in treatment.
So what effect would a dead tooth or missing tooth have on the acupuncture channels? How about a tooth with a low level infection (as is thought with root canals)?
To my knowledge, one knows for sure (i.e. scientifically proven)… but I think it’s safe to say that these factors DEFINITELY have the POTENTIAL to adversely affect the body.
Anti-Root Canal Researchers After Weston Price
Since the Weston Price days, there have been other researchers, dentists, and doctors that have also looked into this issue. One of the most well known is Dr. Hal Huggins… a retired dentist, and outspoken critic of both mercury fillings and root canals.
Dr. Huggins has continued in this line of work by testing for bacteria in and around root canal treated teeth [11]. According to Dr. Huggins, the blood around extracted root canaled teeth can harbor 400% more bacteria than in the tooth itself. Using modern detection methods, he’s been able to identify up to 83 different bacteria in parts of the root canaled teeth.
However, this information hasn’t been published in scientific journals, to my knowledge.
So again, the main argument here is whether or not a root canaled tooth can be sufficiently disinfected during the procedure, and remain disinfected over time.
The anti-root canal camp says NO….
The pro-root canal camp says YES…
Let’s look into some of these arguments in favor of root canal treatment (and their inherent flaws.)
Root Canal Danger Myths?
“Conventional” dentists and endodontists oppose the idea that root canals pose any issue at all. Here are the most common arguments in favor of root canal treatments…
According to the American Association of Endodontists [12]:
- There is no valid, scientific evidence linking root canaled teeth to disease elsewhere in the body.
- “…the presence of bacteria [in a tooth] does not constitute “infection” and is not necessarily a threat to a person’s health. Bacteria are present in the mouth and teeth at all times, even in teeth that have never had a cavity or other trauma.”
- “Tooth extraction is a traumatic procedure and is known to cause a significantly higher incidence of bacteria entering the bloodstream”
- “As recently as 2013, research published in JAMA Otolaryngology—Head & Neck Surgery, found that patients with multiple endodontic treatments had a 45 percent reduced risk of cancer [13].”
I try to approach this debate from a balanced perspective. So in favor of the pro-root canal argument… I also found a study showing no correlation between root canaled teeth and c-reactive protein [14] (an indicator of inflammation.)
In fact, people with greater than 3 root canals, had lower levels of c-reactive protein than people with less than 3 root canaled teeth.
However, the biggest problem with this study is that it doesn’t look specifically at people who have no root canaled teeth at all. The authors themselves state that a conclusive study would have to look at root canal vs no root canal treatment, in relation to c reactive protein and cardiovascular disease outcome.
I would also add that the results may be confounded (clouded) by the number of missing teeth a person may have (more on this later.) Though difficult to measure, how promptly a dental infection was treated could also be an important factor.
How long was tooth infected before it was pulled out?
Was it pulled out right when the infection got into the tooth pulp? Or was it pulled out 6 months after an abscess developed?
Because, the longer you leave the infection in place, the more bacteria, endotoxin, and inflammation you’d be exposed to over time. Endotoxin exposure may also decrease the ability of your body to detoxify it self optimally [15].
Most importantly, the more missing teeth a person has, the greater the chance that this could have happened.
Ultimately, we’d really need a study looking at people with, and without root canals… And in an ideal world, these people would still have most of their teeth.
So as you can see, the arguments for and against root canals can get quite complex. But now that you have a better idea of the issues being argued here, let’s look deeper into the problems with these arguments.
Problems with the “Official Story” …
Though I try to be as unbiased as possible, there are some big issues with the “official story” (i.e. that root canals are totally ok). As we mentioned before, the American Association of Endodontists says:
“There is no valid, scientific evidence linking root canaled teeth to disease elsewhere in the body.”
As you will see… this is just incorrect.
If they said there isn’t any “conclusive evidence”… I’d maybe agree. But to say that there is no valid evidence at all is misleading. For example…
Root Canals Linked to Heart Disease?
A 2010 study from the University of Iowa College of Dentistry showed that people with 2 or more root canaled teeth had 62% greater odds of having coronary heart disease [16]. Interestingly, this only applied to people that had 25 or more teeth.
People with 24 or less teeth didn’t show any difference in risk, from their root canaled teeth. As we mentioned earlier, people with more missing teeth are more likely to have been exposed to the toxic byproducts of infection… namely “endotoxin.”
This study above was a “retrospective cohort study” to look at potential risk factors for disease (prognostic study). So from out of 5 possible levels of evidence (1 being the strongest), this study is level 2 evidence`[17].
A Doctor’s Own Case With Root Canal and Chronic illness
In another example… a group of 3 doctors from the Netherlands published a case study in 2002, explaining of one of these doctors’ own experiences with his root canal treated teeth [18].
Mind you, all 3 of these doctors are dual MD and PhD professors at their universities, including one in rheumatology and another in immunology. So even more so than most doctors, they also have formal training in scientific study.
This doctor could trigger his rheumatoid arthritis just by biting on something hard, using the root canal treated teeth. His symptoms would flare up 1-2 hours after biting on the tooth, and would last for a few hours. This effect was consistently reproducible, which is what caused them to suspect the root canaled teeth in the first place.
When he had his dentist check the root canaled teeth, no problems were found. There were no noticeable issues clinically, or when examined with x-ray. But because of this reproducible aggravation in his symptoms, he had the tooth pulled.
After the tooth was extracted, they found a “thin layer of pus” covering the very tip of the tooth’s root (apex). This initial extraction also caused his arthritis symptoms to subside for a few months.
But after this period of relief, his symptoms flared up again (he still had 3 more root canaled teeth in his mouth). So he had the rest of his root canals pulled. All of these teeth also had a layer of pus at the tip of the root.
Ultimately, removing all his root canaled teeth (along with 3 years of taking aspirin) resulted in 16 years without any recurrence. Interestingly, this doctor’s mother and grandmother had the same exact issue, and were also able to recover after their root canaled teeth were removed.
Overall in terms of being “valid scientific evidence…” this example is just a “case study” (or closer to a “case series,” considering the doctor’s relatives). This is one of the lowest levels of evidence in science [19].
Although a study like this can’t be used to make a broad statement about root canals and overall health… it shouldn’t be disregarded either. This is especially true when you consider the credentials of the authors. Rather, it should inform us that this type of phenomenon is possible, and should be considered when evaluating our own individual situation.
Bottom Line: There IS scientific evidence linking root canal treated teeth to disease elsewhere in the body.
Researchers Find Infected Root Canal Treated Teeth (The Smoking Gun?)
So as we mentioned earlier, biological dentists like Hal Huggins have found high concentrations of bacteria in and around root canal treated teeth. In response to this, the American Association of Endodontists, states:
“…the presence of bacteria [in a tooth] does not constitute “infection” and is not necessarily a threat to a person’s health. Bacteria are present in the mouth and teeth at all times, even in teeth that have never had a cavity or other trauma.”
This statement doesn’t really address the issue. Certainly there is bacteria in the mouth and teeth at all times… But the issue here is the type of bacteria, and the amount of bacteria present.
When you have an infection in an untreated root canal for example, the low oxygen conditions favor (more dangerous) anaerobic bacteria over aerobic bacteria [20]. One study also showed that root canaled teeth are also less resistant to bacterial invasion compared to live teeth [21].
But take a look at what some endodontic researchers themselves have stated about root canal treatments. Below are some quotes from researchers at the Academic Centre for Dentistry in Amsterdam [22]:
- “ …it is likely that current sampling techniques only identify organisms in the main branches of the root canal system whereas it is unlikely that they can sample areas beyond the apical end-point of preparation and filing, or in lateral canals, canal extensions, apical ramifications, isthmuses and within dentinal tubules. Thus, it may be impossible by current techniques to identify residual post-treatment root canal infection.”
GW Comment: In other words, there are a lot of “nooks in crannies” in a tooth. So you couldn’t know for sure if you got all the bacteria or not (with techniques used up until 2006).
- “There is no in vivo evidence to support the assumption that these bacteria can be entombed effectively in the canal system by the root filling and thus be rendered harmless. As a consequence of this residual root infection, post-treatment apical periodontitis, which may be radiographically undetectable, may persist or develop as a defence mechanism to prevent the systemic spread of bacteria and/or their byproducts to other sites of the body.”
GW Comment: In other words, if you don’t kill all the bacteria in the tooth… there’s no good evidence that they can be fully sealed in the tooth either. This may cause an infection that’s clinically undetectable.
- “In two studies where the relationship between histologic and radiologic signs of inflammation was determined in human cadavers, the negative predictive value of radiologic inflammatory signs was 53% and 67%, respectively (Brynolf 1967, Barthel et al. 2004).”
GW Comment: So, if an x-ray shows no infection in your root canal treated tooth, there’s still about a 60% chance that there is a low level infection there. The only way to know for sure would be physically examine the tissue.
- “Histologic observation of root apices with surrounding bone removed from either patients or human cadavers has demonstrated that post-treatment apical periodontitis is associated with 50-90% of root filled human teeth.”
GW Comment: When researchers examined the actual tissue (rather than x rays) under the root canal treated teeth, 50-90% of them showed signs of infection (in various studies.) This quote speaks for itself. No matter how clean a root canal treated tooth could theoretically be… MOST of them have infections in reality.
- “In an in vivo histological study by Ricucci & Langeland (1998), the root apex and periapical tissues were examined histologically following root canal treatment. A strict aseptic technique was applied… At the end of the observation period, despite the fact that 18 (82%) of the 22 roots did not have an apical radiolucency, only three (14%) of them were free of inflammatory cells within the surrounding bone or fragments of periodontal ligament attached to the extracted roots (Ricucci & Langeland 1998).”
GW Comment: So based on one study of carefully done root canals (using techniques available in 1998) there’s an 86% chance of residual infection. And most of these would not be detected by x-ray.
- “From the above it is concluded that histologically, post-treatment apical periodontitis is likely to be present in more than half of root filled human teeth.”
GW Comment: So considering all the different studies they analyzed, these researchers concluded that there’s a greater than 50% chance that your root canal tooth has some level of infection.
- “Thus, if the objective of root canal treatment is to eliminate apical periodontitis at a histological level, current treatment procedures are inadequate.”
GW Comment: So while a root canal treatment may “solve the dental problem”, it often results in some level of infection at the root of the tooth.
So the possibility of of residual infection in root canal treated teeth is the main issue… and it’s likely to be a problem in over 50% of root canal treated teeth.
Now to be fair, these researchers did cite a small percentage of root canal treated teeth that remained without infection. And there are a lot of factors that could give you a better idea of whether or not your root canal treated tooth may be harboring infection… We’ll discuss this in greater detail in a minute.
Is Tooth Removal More Traumatic Than A Root Canal?
So we know that root canal treated teeth have a high chance of being infected, even when x-rays show no infection. But just to be thorough, let’s address some of the other opinions from the pro root canal camp.
Rather than performing a root canal procedure, the solution proposed by the anti-root canal camp is to extract the infected tooth. In response to this, the American Association of Endodontists, states:
“Tooth extraction is a traumatic procedure and is known to cause a significantly higher incidence of bacteria entering the bloodstream.”
Though this may be the case, it also doesn’t address the main issue. The problem here is short term exposure to bacteria via extraction… vs… the potential for long term exposure via root canal.
With an extraction, your body may need to fight off the bacteria released by the procedure (often with the help of antibiotics).
But if over half of root canaled teeth are indeed harboring infection, then your body would have to fight that for years, even decades.
Do Root Canals actually PROTECT YOU from cancer?
Many people in the anti-root canal camp say that root canal treated teeth cause cancer. In response to this, the American Association of Endodontists, states:
“As recently as 2013, research published in JAMA Otolaryngology—Head & Neck Surgery, found that patients with multiple endodontic treatments had a 45 percent reduced risk of cancer.”
Though I think this is an important piece of research… it’s definitely not as cut and dry as it may seem.
First… A “45% reduce risk of cancer” sounds huge. But when you look at the statistics in this study, this “protective effect” is only borderline significant at best.
Second… The people with cancer in this study also had an average of 18-19 teeth (i.e. they were missing 13-14 teeth). The people without cancer (controls) had an average of 23-24 teeth (i.e. they were missing 8-9 teeth). Considering the previous study linking heart disease to root canals… we don’t know what we’d find if we only looked at people with more than 25 teeth (with and without root canal treated teeth.)
And though there wasn’t a clear link found in this study (for one specific type of cancer), another study did find a link between missing molars and an increased risk of cancer overall [23]. As we mentioned before, this could be caused by increased exposure to bacteria and inflammation resulting from past dental infections.
Lastly… This “borderline protective effect” only applies to head and neck squamous-cell carcinoma… not necessarily cancer overall as the quote above implies.
A compelling study would have to look at relationship between root canals and other types of cancer in other areas of the body also.
This would be important, as doctors like Josef Issels MD (Issels Immuno-Oncology), and Thomas Rau MD (Paracelsus Clinic) have claimed a very high percentages of root canaled teeth in their cancer patients [24][25][26].
Considering all of these things, I’d say that the evidence is still inconclusive.
This is also why people should be evaluated on a case by case basis.
Weston Price’s Experiments Misinterpreted
While I’m all for reasonable criticism, it seems that Weston Price’s work on root canals if often misunderstood.
Here are some more arguments from a root canal advocacy website (presumably written by a dentist/ endodontist) [27]. These quotes are referring to Weston Price’s experiment’s of implanting root canaled teeth into rabbits. Below each quote is my commentary/ rebuttal.
Argument 1: “The implanted tooth consisted of a poorly done, failing root canal which was covered in saliva, plaque and tartar into a rabbit, and it developed “crippling arthritis”(like the patient), sepsis, and died. Big deal.”
GW Comment: I’m not sure when this dentist/ endodontist got the idea of a saliva covered tooth. Apparently, Weston Price chemically treated the root canaled teeth before implanting a fragment of the tooth into the rabbit. And even if it was a failing root canal (which is an assumption, though reasonable), it was still chemically treated after extraction. So this is a major misrepresentation of Price’s work.
Argument 2: “Dr. Price was not able to recognize the result of his most amazing experiment was due to the bacterial film surrounding the tooth.”
GW Comment: This doesn’t address Weston Price’s finding that healthy teeth fragments (presumably also covered in some bacterial film) did not cause the same issues in the rabbits. The only way this statement would be relevant, is if he/she is referring to bacterial film inside the infected root canal (if it wasn’t properly cleaned.) In this case, it would also be important to know how Price treated the teeth after they were extracted, and specifically with which chemicals.
Argument 3: “Additionally, the human tooth relative to the size of the rabbit would be like taking anything the size of your forearm, coating it in plaque, saliva, and calculus, implanting it in your back under non-sterile conditions, then developing infection and dying.”
GW Comment: According to Hal Huggins, Weston Price implanted root TIPS into the rabbits… not whole teeth [28]. Additionally, this doesn’t explain why the healthy tooth fragments did not cause any issues.
Argument 4: “Lastly, yet most importantly, root canal treatment back then consisted of wedging an orangewood stick or a heated wire into the canals in a tooth and calling the treatment finished. Well, the infection definitely persisted because sterility was not understood, no antibacterial irrigants or medications were used inside the tooth during root canal therapy, no rubber dams were used to prevent oral bacteria and saliva from contaminating the tooth DURING treatment, no surgical operating microscopes were used to find all the canals, poor restorations were used that never sealed a tooth and instead leaked like a sieve, etc. It is so completely different now.”
GW Comment: This seems to be a fair statement to me. However… according to Dr. Huggins, Weston price took the extracted root canaled teeth first, then chemically treated them with chemicals that were too strong for use in patients [29]. So this statement wouldn’t apply to Weston Price’s experiment.
The only idea that could is worth considering in this statement, is if Price (or the person who did the root canal originally) didn’t use a microscope to thoroughly clean out the biofilms inside the root canals. This could make it easier for the bacteria to survive Price’s subsequent chemical treatment [30].
Argument 5: “Comparing Dr. Price’s antiquated experiment with a SAMPLE SIZE OF ONE, with modern treatment is akin to comparing “bleeding” patients in order to treat “wasting disease” with modern antiviral therapy to combat HIV.”
GW Comment: Though these were animal studies, Weston Price apparently did this experiment with 4000 teeth [31] and upward of 60,000 rabbits [32]… So this much more than a sample size of one.
Furthermore… a treatment technique isn’t necessarily “useless” just because it’s old. Traditional Chinese doctors for example, were using herbs with known anti-depressant effects [33] for over 2000 years, while doctors in the 1930’s were using pre-frontal lobotomies to treat mental disorders [34]. So whether a treatment is useful or not, should be looked at on a case by case basis… not determined by its age.
Argument 6: “For every one person who had “complete recovery” following removal of a root canal treated tooth, there are 1,000’s that had a tooth removed and no resolution of cancer, arthritic conditions, epilepsy, Parkinson’s, etc. Now they still have the disease AND they must decide what to do to replace that tooth with significantly more expensive options.”
GW Comment: I don’t see any evidence to support this 1000’s to 1 statistic… And I would never expect a “complete recovery” from improving just one variable. But I do think the point is still valid. This is why people need to be informed that their root canal could be a contributor to their problem… but that it may also not be. They should also be fully informed of the potential costs, especially if the removed root canal doesn’t help them at all.
But even if a small percentage of people make a dramatic recovery from a root canal removal (like the doctor in the case study above)… Shouldn’t people be aware that it COULD be a possibility? So that they can make their own informed decision? I think so…
Here’s What The Anti-Root Canal Camp Overlooks
Now as you can probably tell, my opinion on the topic aligns much more with the anti-root canal camp. But here are some things that still need to be pointed out…
The Anti-Root Canal Samples May Be Skewed
When you look into the information against root canals, you’ll see very high percentages for the instances of bacteria in these extracted teeth.
One of Weston Prices’ studies for example, found only 10 out of 1000 extracted root canaled teeth remained sterile after incubation [35]. Hal Huggins’s upwards of 92% of sample to be infected with health threatening strains of bacteria [36].
But to be fair, many of these teeth were likely extracted from people that were having health issues already. This is what often drives people to suspect their root canals in the first place.
If a person with root canaled teeth has no health issues at all, she is not as likely to have their tooth extracted for examination.
And the previous study we cited found between 10-50% of root canals with no infection when extracted from a more balanced sample population (i.e. not just people with chronic illness). So the percentage of healthy root canal treated teeth is likely a bit higher than what’s claimed by the anti-root canal camp.
Overall, the chances of having a non infected root canal is still quite low (i.e. an average of only 30% chance). And this is only looking at the root tip of the tooth. A higher percentage of bacterial burden may be found if the entire tooth were considered.
So if there’s about a 30% chance that your root canal treated teeth is more or less “safe”… what factors should you consider about your root canal treated teeth?
The most important is whether your root canal treatment was done well, or not.
Quality Of Root Canal Treatment Matters (But Many Are Poorly Done)
This brings us back to the root canal advocacy site that we cited earlier… And this dentist/ endodontist gives us some very important insight about the difference in quality between root canals [37]. Here’s are some quotes, with my comments below…
Quote 1: “So often root canal therapy is performed poorly, notably by non-specialists. Entire roots go untreated which ALWAYS leads to abscess development. Dentists are taught to use rubber dams, but many never do! Canals are routinely missed or only partially cleaned. I routinely treat these teeth and the infection completely resolves.”
GW Comment: So apparently, “less than adequate” root canal treatments are quite common. And while a poorly done root canal treatment may be bad, it may not even be the biggest worry. Why? Because at least a poorly done root canal would cause an acute problem that you’d clearly notice. What’s even more dangerous is a root canal that is done poorly, but just good enough that it doesn’t create any major problems. And we know from the previous study, an infection that is “completely resolved” on x-ray could still be there in actuality. This brings us to the next quote…
Quote 2: “The real problem with root canals is NOT the treatment itself; the problem is if the treatment is completed poorly, and beneath the standard of care. Rubber dams not being used = allows saliva and oral bacteria into the tooth during treatment. A lack of antimicrobial irrigants, which are necessary to kill bacteria, = allows for persistent infection. Poor obturation (root canal filling) = leads to either nonexistent or deficient sealing of the root canal system which in turn allows for leakage. No smear layer removal = leaves behind bacteria, etc.”
GW Comment: So regardless of who is correct about the root canal debate… you may still have a poorly done root canal. Let’s say your dentist gets all the main roots, but ignored some of these factors above… This could increase the likelihood of a clinically undetectable infection.
So if you do have root canal treated teeth, there’s a good chance that they treated in a “less than perfect” manner.
My Own Experience With Root Canals
And as we mentioned earlier, 50-90% of root canal treated teeth extracted from patients and cadavers, showed signs of infection [38].
I myself had three root canal treated teeth, and all were done by a general dentist… not an endodontist. When I had them removed, two of the three were obviously infected. And one of my infected root canal treated teeth was “perfectly fine” according to conventional dentistry.
From what I recall, there were also no microscopes used during my original root canal treatments. As you’ll see next, this may be a critical factor.
Accessory Canals Can Be Treated (But Can Easily Be Overlooked)
One of the biggest issues with root canals are the “accessory canals” that branch off of the main root canal. And there are a lot of misconceptions here that need to be clarified.
The anti-root canal camp says that dentists can’t treat these smaller accessory canals in your teeth. This is thought to be a place for bacteria to hide and multiply. They even go as far to say that dentists aren’t taught about these accessory canals in dental school [39].
Well, this only partially correct… However, you’ll see the point they are trying to make is still valid.
Modern day dentists ARE WELL AWARE of accessory canals. And the reality is, root canal specialists can find and treat accessory canals using specialized operating microscopes [40][41].
HOWEVER, this mainly applies to larger accessory canals (apparently)… and general dentists will likely even miss these (as opposed to root canal specialists [42]). AND, as the we talked about earlier, even some endodontics researchers admit that it’s unlikely that you could treat ALL of a tooth’s accessory canals [43].
So while some can indeed be treated… accessory canals are still likely to cause problems in root canal treated teeth (especially if they are grossly overlooked.)
Undetectable Doesn’t Mean Non-Existent
The pro-root canal camp also refers to x-ray evidence as proof of healing after a root canal [45][46]. But as we mentioned before, multiple tissue studies have shown a problem can still exist even if it isn’t detected in one instance of x-ray [47].
Here’s another example from Dr. Tom Colpitts. He explains how switching to a 3D CAT scan has enabled him to find problems with root canals that would have gone undetected on a normal x-ray.
According to him, nearly 70% of root canals show signs of infection (presumably after 10 years).
Dr. Colpitts’s findings also corroborates the other studies cited earlier (i.e. that there’s roughly a 30% chance that your root canal treated tooth is ok.)
So What’s The Full Story?
As you can see, the issue of root canals is much more complex than “all root canals are ok” or “all root canals are bad.”
However… It’s safe to say that the phenomenon of root canals impacting one’s health is a DEFINITE POSSIBILITY, and should be evaluated when looking at your own situation.
ULTIMATELY, root canals may not ALWAYS be a burden to your immune system, but they LIKELY ARE in most cases.
Bottom Line:
- There’s not yet a SCIENTIFICALLY ESTABLISHED link between root canals and cancer. The only indication of a link comes from unpublished clinical observations. But, it’s still a possibility
- Root canal treated teeth ARE likely to be an immune burden, in more than 50% of cases. But this immune burden can happen to varying degrees. This can range from being the main cause of a chronic disease, to likely insignificant… and every possibility in between.
- Root canals overall can range from perfectly done, to totally inadequate… and everything in-between. If your root canal was performed by a very meticulous endodontics specialist, there may be a greater chance of it being ok.
- But overall, the chances that you had a “poorly done” root canal treatment is pretty high. This would increase the likelihood of immune burden on your body.
- The older the root canal treated tooth, the more likely it is to be an issue also.
- Ultimately, how your body is affected by a root canal depends on the degree of the immune burden, in relation to the strength of your immune system.
- But if you are fighting cancer (and want every variable in your favor) you’ll definitely want to consider your root canal treated teeth as a possible source of immune burden.
So Here’s What You Can Do
If you have root canals and are fighting cancer, here’s what you’ll want to consider…
First, decide how important your root canaled teeth are to you. You’ll want to factor in your finances, your ability to handle the stress of the extraction procedure, and your willingness to put up with the alternative option (i.e. denture, bridge, or implant.)
If extraction doesn’t pose much of a problem for you… and you just want to ensure there’s no immune burden at all:
- Have your root canaled teeth extracted by a competent biological dentist. And if they do find evidence of infection, be sure to also share with us in the comments below. This will help to increase awareness about this issue. 🙂
- Consider taking some immune supporting and detoxification supplements before and/ or after the procedure (with permission of your dentist). Things like beta glucan, coriolus versicolor, AHCC, are good options for supporting your immune system.
But if getting your root canals extracted is a burden for you:
- First consider the fact that your root canal has greater than a 50% chance of being histologically infected (i.e. infected, but not visible on x-ray.) The true figure is likely to be around a 70% chance.
- Then find out how old your root canals are. The older they are, the greater the chance of them causing an issue (especially if they are more than 10 years old).
- Find out who did your root canal. If it was done by a general dentist, rather than an endodontist, then there’s a greater chance of it causing an issue. If they used an operating microscope during the procedure, there’s a greater chance of the tooth being ok.
- Have your root canaled teeth evaluated by a dentist or endodontist using newer diagnostic technology (like 3D-CAT scan). In this case, you’ll also want to consider supplements to help reduce the impact of the radiation. These include high quality Omega 3 fats from fish, krill, or algae… liposomal glutathione, curcumin, and polyphenols in general (i.e. resveratrol, quercetin, EGCG).
- Have your physician check your blood for markers of inflammation and infection (though this still may not be conclusive).
- You can also check to see if you can create any symptoms by biting down on the root canaled tooth. Try using it to (carefully) chew on something hard or tough (i.e. jerky, nuts, etc…) Then, note if you get any noticeable symptoms including fatigue, muscle stiffness, pain, swelling, or aggravation of any symptoms that you already had.
- If any of these things above point to a potential problem, there are two possible solutions. The first is to ask your dentist about “apical surgery.” This involves physically inspecting the root of your root canal treated tooth for signs of infection, and treating it if necessary. According to the endodontic researcher that we cited earlier, even this should be done meticulously (using an operating microscope, micromirror, ultrasonic irrigation, and smear layer.) This should allow complete healing in 97% of cases [48].
The other choice (which maybe still safer), is to have your root canaled teeth removed by a competent biological dentist. The reason I say that this may be safer, is that the studies above only looked at the root of the tooth. It’s not clear if there could still be infections around accessory canals higher up on the tooth.
With either choice, I’d recommend consulting with a biological dentist before deciding.
Have you had an experience with root canals in relation to your health? Have you had your root canals removed? Whether extraction helped you or not… let us know in the comments below.
Are You A Candidate For Our Program?
If you’d like to learn more about the AntiCancer360 approach and see if we can help you… please watch our free online webinar to learn more about our approach. Then at the end, you’ll be able to schedule a free call with someone from our team so that we can discuss your case in more detail.
Citations:
Gene Wei is a Board Certified Doctor of Oriental Medicine in the state of Florida, and the founder of AntiCancer360. He’s also a graduate of the University of California Los Angeles, and East West College of Natural Medicine.
His practice is focused on integrative and natural anticancer strategies. Over the years, he’s helped many people overcome difficult cancers… including some cases of “terminal cancer” which were able to be reversed with an “Aggressive Integrative Approach.”